South Sudan: Doctor Recalls Trauma and Triumphs with COVID-19 Patients
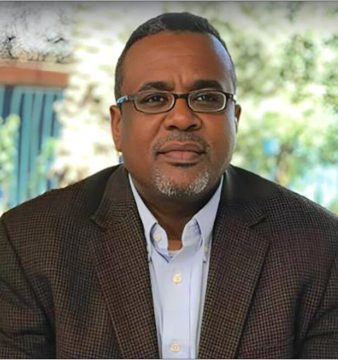
Dr Abe Manase Lori is haunted by the memory of a 45-year-old patient who succumbed to COVID-19 at the beginning of the pandemic in South Sudan.
‘This was a time when we ran out of resources…It was unfortunate. We lost him,’ said the 34-year-old doctor, who works at the Dr John Garang Infectious Disease Unit in Juba.
Since April 2019, conditions have improved. The facility is now managed by International Medical Corps, a global humanitarian organisation that equipped the facility with 60 extra beds, bringing its patient capacity to 84. The renovations also included a temperature-controlled dispensing pharmacy and a fully equipped laundry area to boost infection prevention and control measures.
‘Not having the Dr John Garang Infectious Disease Unit would have been a national disaster,’ said Lori, who hails from Kajo Keji in South Sudan’s Central Equatoria State. He grew up without easy access to healthcare, having spent more than 15 years of his young life as a refugee in Uganda.
Lori said that improvements in the infectious disease unit have made a significant difference. Between April and June 2020, at the height of the pandemic in South Sudan, the recovery rate for COVID-19 patients was 75%. Between July and December 2020, the recovery rate improved to 89%.
The expansion of the infectious disease unit was the combined effort of the Ministry of Health, World Health Organization (WHO), World Food Program (WFP) and International Medical Corps (IMC).
The African Development Bank Group (AfDB) also boosted South Sudan’s efforts to fight the pandemic. In June 2020, the Group’s African Development Fund (ADF) approved a USD4.2 million grant from its Transitional Support Facility. The grant fell under the framework of the Bank’s COVID-19 Response Facility. The funding also enabled the successful installation of the country’s first oxygen plant at Juba Teaching Hospital — a timely project to cater for critically ill COVID-19 patients.
The days are still tough in the wards of the country’s only infectious disease unit. Lori said a typical shift is filled with emergencies and new arrivals.
‘COVID patients are associated with a lot of stress…so you find they are traumatised, they believe they are not going to survive,’ the Juba-trained doctor said. ‘Some of them refuse to be put on oxygen because they think it is a sign they are going to die.’
Many patients refuse to eat or resist being cleaned when they wet their beds. Some are terrified when they see doctors in head-to-toe protective gear, thinking it spells their end. “You need to be understanding,’ said Lori.
However, he also has a good number of uplifting patient stories to share. For example, a 72-year-old man who was diabetic and hypertensive managed to survive the deadly virus after a heavy regime of treatments. “I am so happy that we were able to save him,’ said Lori. ‘And he was able to say thank you for the support you have given me.’
To date, there have been more than 12,900 COVID-19 cases and 133 deaths in South Sudan. The country is one of the countries with the lowest rate of COVID-19 vaccinations in the world. Just 0.8% of the population have had one dose (218,000) and 0.3% have been fully vaccinated (133,000).
This article is by African Development Bank Group (AfDB).