The Sudanese Health System: an overview
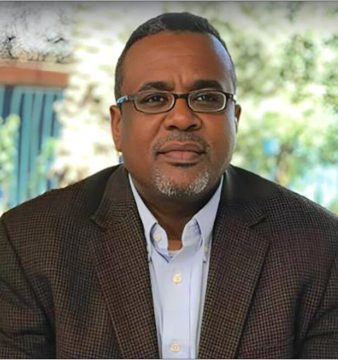
Suzanne Sharief gives an overview of the nature of the Sudanese health system. Deregulation, a cost-sharing policy and the introduction of user fees shape Sudan’s current health system.

An outdoors waiting area for patients at Al Sha’ab Teaching Hospital, Khartoum. (Credits: 500 Words Magazine)
Sudan, once the largest country in Africa, split into Sudan and South Sudan in July 2011 after a civil war that has left both countries in shambles. The different geographies and ethnicities found in Sudan shape the health profile of the Sudanese population. The epidemiological profile of Sudan is somehow typical of a Sub-Saharan African Country, dominated by malnutrition and communicable diseases, frequently aggravated by natural disasters (floods and droughts) as well as sustained internal conflicts. The most prevalent communicable diseases are: food/waterborne diseases, vector borne diseases, water contact disease, and diseases transmitted through respiratory droplets. Malnutrition is a leading cause of mortality and morbidity in the country especially among children. There’s also a lack of capacity deal with the current increase in the prevalence of non-communicable diseases – such as heart diseases and cancer.
The health system in Sudan is complex with countless underdeveloped areas. The Public Health System was historically the only provider of health services. The burden of service provision fell solely on the health system with a minimal role for the community or the clients in the planning process or the quality of the services provided. The government of Sudan has succeeded in providing free health services since the colonial period, through independence and up until the beginning of the 1990’s. However, and like most systems that were put in place during the colonial period, the health system collapsed and the health services available failed to meet the increasing demand of the growing population. Furthermore, the government was faced with several political and economic constraints that resulted in a decrease in the proportion of GDP allocated for health from 1.5% in 1982 to 0.07% in 1990. Up until 1990, the health system had two main obstacles: a lack of medical personnel, and a lack of health facilities. This inference was reached through a retrospective analysis conducted by the Federal Ministry of Health in 2002, which served as the main impetus for the government to approve the establishment of medical and nursing schools in most states throughout the country. This proved cumbersome in more ways than one. First, a lack of qualified teachers meant the medical personnel to come out of these schools were not of the competence level required. Then, with the unsupervised construction of the many medical facilities across the country, new budget issues arose with regards to maintenance, funding and service provision.
The government then started a progressive deregulation of the healthcare system. The Federal Ministry of Health decided to decentralise health services and decrease the regulations that were historically enforced by the Federal Ministry; the difference states were given more authority over their respective health planning. Deregulation also resulted in creating a health services market and competition in the provision of health services. Contrary to common belief about the deregulation of health systems and the introduction of competition there was a decrease in the standards and quality of the health services being provided. There was also an issue with equitable distribution of health services throughout the country, with poorer states receiving the least health services. A major change in the history of health care provision in Sudan was the introduction of the user fee. User fees are charges for health services. They are collected at the point of care as registration fees, consultation fees, or fees for different services; they come directly out of the user’s (patient’s) pocket. The introduction of user fees was found to decrease health service utilisation, especially preventative care services.
As a consequence of the ‘’liberalisation policies’’ the governments’ expenditure in health was significantly reduced. This lead to inefficiency in the utilisation of resources, unequal geographical distribution of health services, general deterioration in the quality of services provided, dissatisfaction of clients and deterioration of the work environment; this lead to a continuous decline in the workforce in the sector. The government had to restore and maintain provision of health services of acceptable quality at a low cost; this would only be achieved with more resource allocation. A Cost-Sharing Policy was introduced in the early 1990’s as one of the components of the economic reform and liberalisation policy. The Cost-Sharing Policy is the distribution of the costs of health services to different entities to elevate the part of the burden bestowed on the user. It is known to minimise catastrophic health expenditure. It is used by health insurance schemes and often has methods, including: co-payment, co-insurance, fixed deductible amount or ceiling.
Subsequent to the decentralisation reform in the 1990s, the health system was then composed of three layers: federal, state and locality. The Federal Ministry of Health (FMOH) is responsible for construction of national health policies and overall health planning, in addition to human resource development and international relations. The FMOH also plays a supervisory role to the affiliated state programs and is mandated to intervene at any stage to deal with emergencies, including epidemics and other health disasters. The state ministries of health are entrusted with the planning, management and delivery of health services in addition to programming and project management at the state level. The Locality Health Department is responsible for management and delivery of Primary Health Care services including environmental health activities.
Currently, the health system in Sudan provides services under two main domains: the curative, and the preventative health services. Each domain has relevant programs that run parallel and provide services at different outlets. One of the biggest challenges within the health system remains to be the number of medical personnel, with only 1.3 health workers per 1,000 population (WHO minimum of 2.3). The disproportionate and irrational human resource distribution and services across the country is also a major contributor to the general dissatisfaction by end users.
The current national strategic plan aims at building a nation with healthy individuals, families and communities with emphasis on the health needs of the poor, disadvantaged and vulnerable populations. Within this broad vision, the health goals should ideally be based on the health challenges facing the country and how to efficiently and equitably address these challenges. However, politics invariably comes into play and the bigger picture is often lost and the all-so-noble vision, mission, and plans become the only new and shiny items in display on the broken walls of our crowded and dysfunctional health facilities. A qualified and conscious leadership can pull the wreckage of this system together and help create a dignified working environment for the service providers, and services as good as can be. Investing in future health policy makers and changers is the key for a better health system and a healthier nation.
Suzanne Sharief, MBBS, MPH, is a seasoned public health professional focusing on reproductive health research, innovative health solutions and health policy.


Let me congratulate Dr. Sharief on her excellent effort on reviewing the Sudanese health system. The endeavor to write in Sudan is heroic and few will do it. I find myself agreeing on most of the findings except two, one historical and the other conceptual.
The historical is that introduction of user fees started since 1978 when Sudan stated to adopt the World Bank prescription, better known as Structural Adjustment. In 1994 the free service – as misleading as it is – was abandoned.
The conceptual comes in the policies to decrease the allocated GDP, which is an ideological choice and a socio-economical bias and not as said by the author. Furthermore, the government was faced with several political and economic constraints that resulted in a decrease in the proportion of GDP allocated for health from 1.5% in 1982 to 0.07% in 1990.
I had finished a book about the Sudan health and would like to discuss more on the issue, my mail is added.
Thank you very much Dr. Amr for the compliments. I am in no shape or form a health economist-I would have been if I wasn’t so intimidated by numbers (smile). I agree about the first point, I had a whole paragraph about the structurally adjusted programs “SAPs” but had to remove that so that the article is not super long. I am glad that this article will start such discussions especially among professionals like yourself.
Well done Dr. Sharief on a brilliant and insightful article! I am also a medical professional currently finishing up my MPH and starting an MSc in University of Copenhagen on Health Services and Disease Prevention, but my interest lies in the former as I find health policy and planning is an integral and contemporary requisite for our failing health system in Sudan. I am very glad I stumbled upon this article. If you don’t mind, I will be in touch on LinkedIn in the near future to discuss some form of possible collaboration in the years ahead to form some kind of leadership that genuinely cares for the health of our fellow Sudanese citizens.
I wish you the best of luck and keep those articles coming!
Kindest regards,
Dr Shehata
Thank you very much. I would love to be in touch.
http://linkd.in/1mwlrWB
Great review of the Sudanese health system, thank you Dr Suzan. I am not a public health professional myself, but having practiced medicine in Sudan I can say that, indeed, the health system is underfunded, understaffed and, most importantly in my opinion, inadequately supervised. The training system for medical staff is lacking in more domains than one, and continuous education is either absent or poorly organized.
Also, non-communicable diseases seem to be a growing issue in Sudan; everything from cancer to neurodegenerative disease are steadily becoming a burden that the health system may not be able to deal with in the future – their management is expensive, cumbersome, and requires specialist care.
I totally agree. Thank you for the insightful comments.
Dear Ms. Sharief
Thanks for this interesting study. Do you have or suggest any site to help me understand better the eye medical status in Sudan? I would appreciate if you can help and guide me in researching this industry especially from a business point of view. I really appreciate your help. Thanks